CRISPR is a scientific breakthrough that is going to change our future. It is a gene editing tool that can easily be used in any modern biology lab; it is more economical than any technology that came before it; and it can target any gene, both in a dish and in living organisms, and edit it with pinpoint precision, allowing researchers to systematically alter genes or turn them on or off.
Naturally, the scientific community is excited about all the doors CRISPR will open. CRISPR will help researchers understand the roles of specific genes, and how they behave in health and disease. Not only that, but it will be possible to treat any disease with a genetic basis, from cancer to HIV/AIDS, by editing the genomes of living people. CRISPR is already helping agricultural scientists engineer hardier crops, and has helped biologists create a malaria-resistant mosquito in the lab, complete with a mechanism that could be used to propagate the change through the entire species.
But the fact that something is possible doesn’t mean that we should go through that door. There may be unintended consequences, and edited genes can potentially be inherited, raising important and urgent ethical questions. Defining boundaries keeps research ethical and safe, which is why researchers from across the globe are meeting this week to discuss the safe and ethical limits of human gene editing.
What is CRISPR?
Genome editing with CRISPR-Cas9
Animation courtesy of the McGovern Institute for Brain Research at MIT
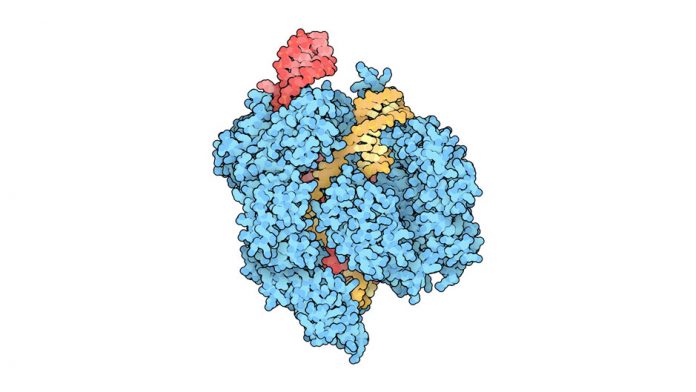
CRISPR and Cas9 proteins work as a pair, and were originally a defense mechanism found in bacteria. When a virus infects a cell, CRISPR/Cas9 hunts down the foreign DNA and makes a cut to disable it before it can do harm.
The CRISPR/Cas9 complex unzips DNA and then runs down its length searching for a matching target to a piece of guide RNA. Once found, Cas9 acts as a pair of molecular scissors, cutting the target in a precise location. When the cut ends are repaired, there is an opportunity to alter the gene sequence, either by turning the gene on or off, or by splicing in a new piece of genetic code.
To change the identity of the target gene, only one piece of the system needed to be updated: the guide RNA being used by the complex.
But CRISPR/Cas9 was not specific enough – up to 5 of the 20 letters in the guide RNA could be a mismatch and Cas9 would still make the cut, resulting in a high error rate and many off-target mutations.
More recently, researcher Prof. Feng Zhang at MIT tweaked Cas9 to improve its specificity, leading to an error rate that is now comparable to the spontaneous mutation rate in humans.
How can CRISPR be used to find new cancer treatments without changing the genes of living patients?
CRISPR technology can be used to identify new drug targets
Animation courtesy of AstraZeneca
It’s amazing to think about how little we know about how genes work. They have complex interactions. There are many genes that stay inactive. It’s been 15 years since the full human genome was first published, but until now we haven’t had the tools to tease apart which genes are essential.
Cancer is a genetic disease caused by mutations in the genetic code. While directly switching off the genes responsible for cancer may be a long way off, Prof. Jason Moffat and Prof. Stephane Angers at the University of Toronto has found a way around this: his group published a study in Cell last week where they systematically turned off 18,000 genes in cancer cells one at a time to find out which ones were essential to their survival – that’s 90% of all human genes.
By comparing these results against the essential genes in healthy cells, new targets for cancer treatment were identified – ones that are essential to cancer cells, but that healthy cells can do without.
The hope is that there are many essential genes that are specific to cancer cells, and that drugs can be developed to target them. This approach has already uncovered that a common diabetes drug, metformin, can kill certain cancer cells in the lab – a connection that could never have been predicted.