Open heart surgery is a relatively new field, dating back to the early 1950s. But even in this short span of time, advances have been enormous: heart surgery has gone from being extremely risky to safe and almost commonplace. And Canadian surgeons have played a key role in this transformation.
Let’s take a look at how the cardiac operating room has changed over the years.
You’re lying on a stretcher being wheeled down a long, white corridor. Lights flash above you. There is a breathing mask on your face, sending extra oxygen to your lungs, but your chest still hurts. It must be your heart again. A doctor says they’re bringing you to the operating room.
It’s:
1955
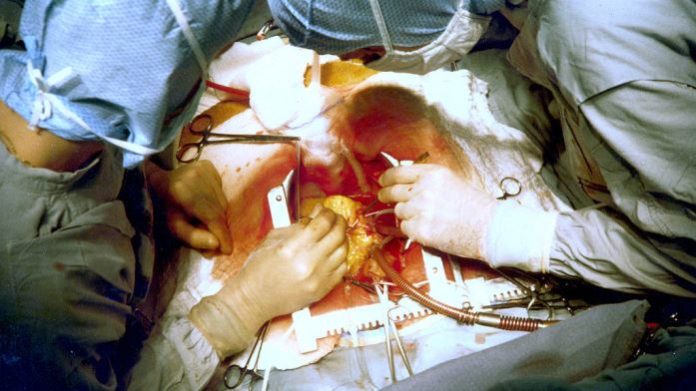
Inside the operating room, several nurses wearing white gowns stand around what appears to be a large table packed with crushed ice. A stainless steel machine the size of a large radiator sits beside it, tubes protruding from its top and sides.
The doctor explains that in order to give them more time during the operation they have to cool your body down. The colder your body, the less oxygen your brain and other organs need, allowing the heart to be stopped for longer before any negative effects appear. A Canadian surgeon named Wilfred Bigelow at the Banting and Best Institute in Toronto figured this out after a fascination with groundhog hibernation, where their bodies remain at 4°C for extended periods of time with no visible damage.
And don’t worry, he adds, clotting won’t be an issue because they’ve injected a dose of heparin into your bloodstream. Heparin prevents blood clots that could otherwise lead to complications. It was first used clinically by Dr. Gordon Murray at the Toronto General Hospital almost twenty years back.
Unfortunately, they don’t have the heart-lung machine set up yet, the doctor says, pointing at the large contraption. This machine would allow your blood to bypass the heart where it would be reoxygenated and recirculated throughout your body, buying the surgeons even more time to perform the operation with a clear field of view. Just wait, soon machines like this will make ice bath cooling a thing of the past!
But back to your surgery. The procedure is expected to take all day and your chances of survival are about 50%.
You hope for the best and count backwards from ten as the anesthetic begins to take effect: ten, nine, eight…
2015
The operating room is brightly lit by several adjustable lamps, almost like at a dentist’s office. Tables covered in blue sheets are filled with stainless steel instruments and piles of white sponges.
The doctor explains that you are too high risk for open-heart surgery, but they can replace your aortic valve without opening the chest using the TAVI (transcatheter aortic valve implantation) procedure, established by Dr. John Webb at the University of British Columbia. They’ve injected a fluorescent dye into your blood so that they can visualize the blood vessels using a large machine set up beside the operating table.
They’ll thread a new valve through the femoral artery from just above your groin all the way up to your heart. They’re using a stentless valve that can be inflated once positioned at the right location in the heart. The lack of stent – a supporting meshwork – allows for smoother blood flow after the operation. Valves like these were made possible by the pioneering work on stentless porcine valves of Dr. Tirone David, a cardiac surgeon at the Peter Munk Cardiac Centre, part of the University Health Network in Toronto.
The procedure shouldn’t take more than a few hours and risk is minimal, but you’ll still have to stay in the hospital for a while to recover after surgery.
Seven, six, five…
The not too distant future
The doctor explains that they’ve received cardiomyocytes, heart muscle cells, from a cell bank and will inject them into the heart muscle that was damaged after your latest heart attack. These cells will regenerate the damaged muscle and restore your heart function. Heart interventions are no longer purely mechanical, she says, they’re now able to change the biology too!
Initial cell therapies for the heart were based on stem cells and were more about boosting the performance of surviving cells. Clinical trials for such procedures were done right here, at the Peter Munk Cardiac Centre by Dr. Terrence Yau, she beams. But now, they’re not only improving outcomes after heart attack, they’re actually reversing the damage.
The procedure will only take a few hours, and thanks to advances in recovery methods, you should feel great in much less time.
Four, three, two, one.
Almost every aspect of heart surgery has changed since it was first attempted, says Dr. Tirone David, and often due to Canadian inventions and techniques.
“Canada has a rich heritage in cardiac surgery. Canadian heart surgeons continue to introduce new approaches to treat patients with heart diseases and remain in the forefront of research in development in this area.”