Your oncologist bursts into the room in a whirlwind of papers and quickly sets about checking on your progress. How is the treatment progressing? What are the latest test results? Is the tumour shrinking as expected?
Against that flurry of activity, and the focus on battling your cancer, it can be very hard to talk about your difficulty sleeping, nausea, or feelings of depression. And is the breakdown of your marriage from the stress of treatment something you can even talk to a doctor about?
Holistic care—viewing the patient as a whole and improving their overall well-being—is an important goal of modern patient-centred care, but it’s hard for a doctor to find time or remember to check for every possible issue at every clinic visit. Patients often have trouble broaching certain topics, fearing that the issues are trivial, not a normal part of treatment, or bothersome to their busy doctors.
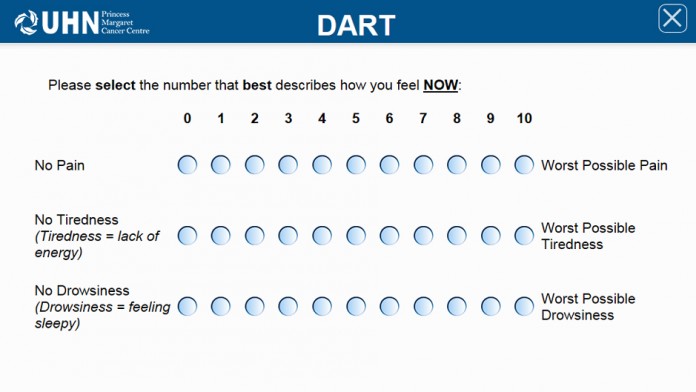
To solve this, Drs. Madeline Li and Gary Rodin of UHN conceived of the Distress Assessment and Response Tool (DART), a computerized survey that incorporates several validated questionnaires from the psychological literature. Developed by Tran Truong’s Health Informatics Research (HIR) team at the Techna Institute, DART is now the standard-of-care at the Princess Margaret Cancer Centre.
Personalized plans for cancer care involve more than just tumour response to treatment
Video courtesy of Cancer View Canada
Every time a patient comes in for a clinic visit, they fill out a short survey on a touch-screen computer or iPad that assesses all aspects of their progress and well-being, including physical symptoms, practical concerns, and emotional state—not just their cancer. Covering aspects of a patient’s life that may not be covered in a typical exam or clinic visit, such as anxiety and distress, helps inform the care team of any developing issues, and enables them to intelligently integrate psychosocial support and palliative medicine to control symptoms.
Having an electronic record of a patient’s symptoms, tracked over a period of time, also helps health care providers better assess a patient’s therapeutic progress.
DART has been such a success at Princess Margaret that it is being licensed to other health systems—such as the Rossy Cancer Network in Montreal, a consortium of three hospitals affiliated with McGill University—and translated into other languages.