Researchers behind a new report have detailed the characteristics and patterns of opioid use across the province of Ontario. The Ontario Drug Policy Research Network looked at opioid use throughout the entire population, organizing data to highlight trends according to location, use of health services, and demographics.
Some examples of areas badly hit by opioid abuse and opioid-related deaths include Thunder Bay, north-western Ontario, North Bay, Parry Sound, and Sudbury.
“Our ‘Behind the Prescriptions’ report is significant because, for the first time, it provides a picture of both opioid prescribing patterns across the province as well as people who experience harm from these drugs,” says co-author Tara Gomes.
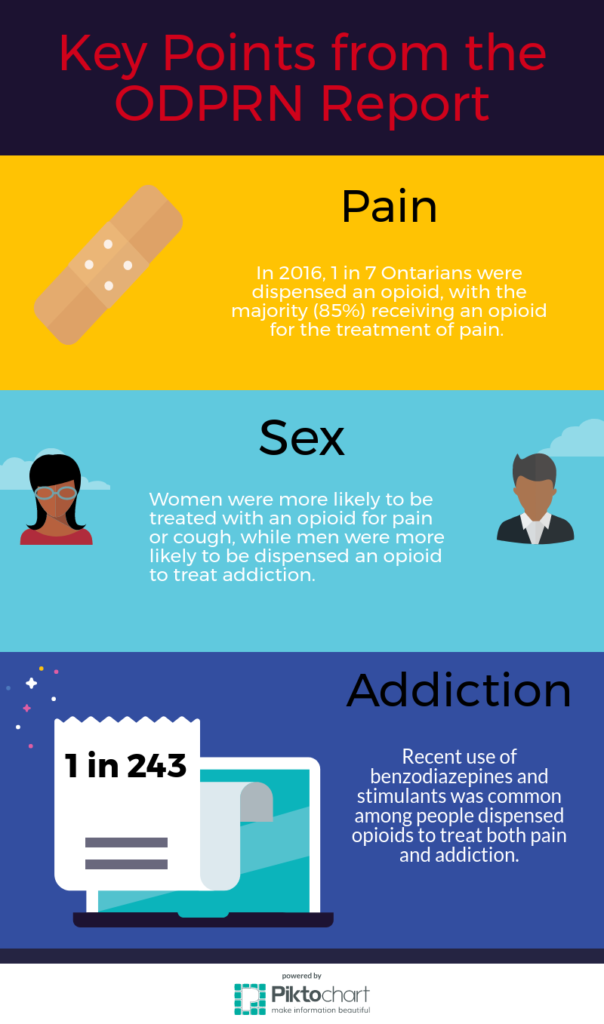
Concern over opioid use in Ontario has been ongoing for over 20 years, and previous studies showed that the rate of prescriptions continues to rise. Co-prescriptions with other drugs such as benzodiazepines increase the chances of an overdose, so easy access poses a serious risk to public health.
Poverty and drug abuse: two sides of the same coin
The report highlights that although liberal dispensation of opioids occurs across all income levels, the basis for a prescription differs greatly according to a patient’s socioeconomic class. One of the most striking figures in the report was that 58.2% of those prescribed opioids as part of an addiction treatment program were from the two lower quintiles of socioeconomic status.
Lower socioeconomic groups are typically predisposed to other negative social determinants, which increase the likelihood of developing an addiction. Unstable housing situations, isolated communities, childhood traumas, and poor education levels often go hand in hand with addiction.
Rural areas were noted as markedly higher than urban areas for addiction numbers. However, such areas had only moderate prescription rates, so researchers pointed the finger at illicitly obtained opioids in these cases.
Compounding all of this is the lack of access to addiction treatment. Areas like Thunder Bay and Haliburton both have high levels of opioid-related deaths, but only the former has high rates of methadone and naloxone, which are prescribed to wean people off the hard stuff. The presence of these drugs is indicative of a functional addiction treatment program, so a lack thereof is symptomatic of an area in need of intervention and greater care.
“I think that [the report] highlights the need to better understand what factors lead this already vulnerable population to be more negatively impacted by Ontario’s current prescription opioid epidemic,” says Gomes. “Specifically, understanding how other social determinants can influence this issue may help ensure that policy responses are appropriately tailored to the needs of this population.”
In pain? Here, take this pill…
Although addiction and overdoses take the lion’s share of concern, it’s also worthwhile looking at pain and cough-related opioid prescriptions. Addiction has to start somewhere, and even though there are a myriad of ways this can happen, treating pain via a prescription is a common one.
“We know that not all people will become addicted to opioids, but there are certain people who are more vulnerable to developing an opioid use disorder,” says Gomes. “So, with high prescription rates at the population level, we increase the chances that they will be exposed to an opioid, putting them at risk of addiction and related future adverse consequences.”
In 2012, the Narcotics Monitoring System was launched by the provincial government to monitor and account for all opioid prescriptions. The idea was to gather data on the patterns of use so physicians could make better informed decisions about prescriptions.
By 2015, a number of public health initiatives were launched to encourage safer prescription practices because of worrying rates of use. In 2015, 1 in 7 Ontarians used opioids to tackle pain. In 2016, this number fell back to 1 in 8. The authors claim that there could be a link between these initiatives and declining prescriptions, though 1 in 8 is still far too high.
With this report, policymakers now have the most detailed information yet to track and identify the channels exacerbating Ontario’s opioid crisis, and well-informed policies are often a tipping point towards improvement.