When diagnosed with a bacterial infection, patients want to be treated quickly with an antibiotic that will work. But it’s not always that simple.
Once a blood test has been administered, it could take up to five days for a lab to figure out what type of infection a patient has. It’s only then that a doctor can explore which antibiotics the infection will respond to best; this is also known as the infection’s antibiotic susceptibility, and its assessment is becoming more important as antibiotic resistance rates continue to rise.
If the infection is serious, this is time a patient might not have, as each hour treatment is delayed increases mortality rates by nearly 8% due to infection complications.
Now, researchers from the University of British Columbia – Okanagan and the University of Calgary have developed a biosensor that provides accurate and reliable diagnosis of a bacterial infection almost instantly. With further development, this could provide healthcare professionals with a portable and inexpensive biosensor for use during patient consultations, even in rural or remote settings.
But how does it work? A patient sample is passed through tiny tubes in the hand-held biosensor and exposed to microwaves. By analyzing the resulting electrical signal, the ‘lab-on-a-chip’ is able to generate a profile of the bacteria present. Changes in the sample (for example, rapid bacterial growth) in turn cause almost immediate changes in the electrical signal, indicating growth, or how the bacteria respond to treatment with various antibiotics.
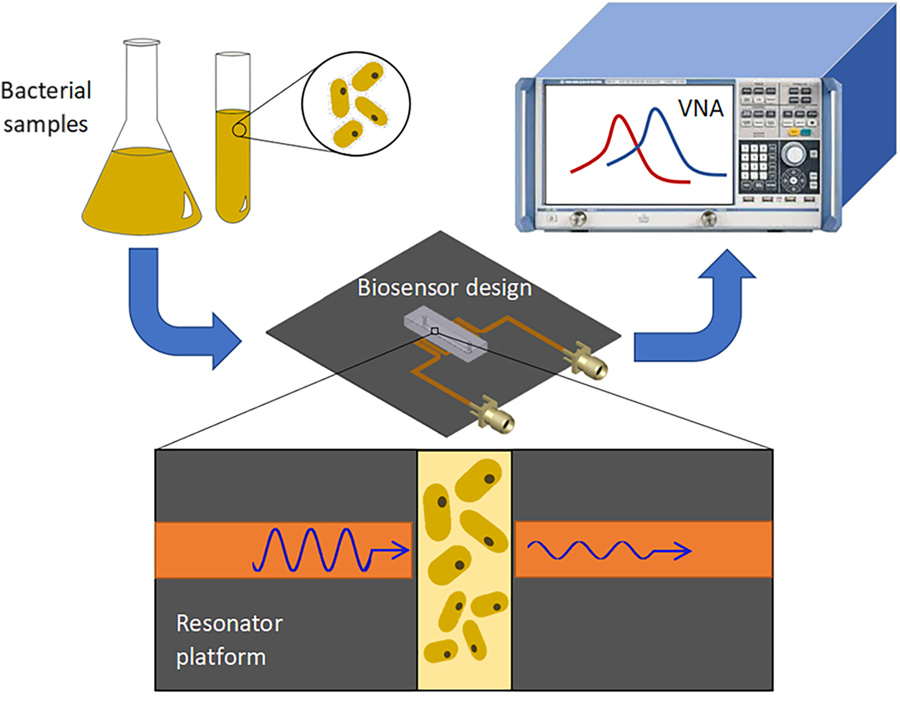
The current proof-of-concept study used E. coli bacteria as a test sample, but the biosensor has the potential to perform real-time diagnosis of many infections, and their antibiotic susceptibility, at the point-of-care. This is in stark contrast to current bacterial detection methods that rely on large and expensive instruments, and laborious processes, without potential for miniaturization.
“The device is able to rapidly detect bacteria and, in addition, it screens the interaction of that bacteria with antibiotics,” explains Mohammad Zarifi, an assistant professor at UBC Okanagan, one of the team who developed the device.
“The combined results give healthcare practitioners more information than they currently have available, helping them move forward to determine accurate treatments.”
Although there is still work to be done, this biosensor is a significant step forward in improving how we diagnose and treat bacterial infections, and could be an invaluable tool in the fight against antibiotic-resistant infections in hospitals and the community.