For women under 65, it’s essential to be routinely screened for cervical cancer. This is typically performed using the standardized Pap smear, but more and more evidence suggests that the HPV test may be a superior form of screening.
Now, Canadian researchers may have solidified that idea with a randomized clinical trial involving over 19,000 women from British Columbia. Published in JAMA, the paper reported that the HPV test could detect precancerous cells earlier and more accurately.
HPV: The ‘common cold’ of sexually-transmitted diseases
The Human Papillomavirus (HPV) is extremely common (around 80 million Americans carry it) and is the basis of 99% of cervical cancers. It’s usually eliminated by the immune system, but if this fails, the virus can cause cellular changes that develop into precancerous lesions, setting the stage for cervical cancer.
Some 1,550 women were diagnosed with cervical cancer in Canada last year, and approximately 400 died from the disease. Cervical cancer is highly preventable, however – the Centers for Disease Control estimates that 93% of cases are preventable.
The first line of defence is the HPV vaccine, a powerful – though not absolute – deterrent for the disease. Unfortunately, uptake for the program can be challenging because it works best if administered to children before they become sexually active, and this can be problematic for several reasons.
Discussing children’s sexual behaviour with parents can be taboo subject matter. Cultural or religious influences aside, some parents mistakenly believe that the mere act of discussion encourages sexual activity.
The next step is routine screening. The Canadian Cancer Society recommends that women aged 21+ should book an appointment at least once every three years to catch it early in its development.
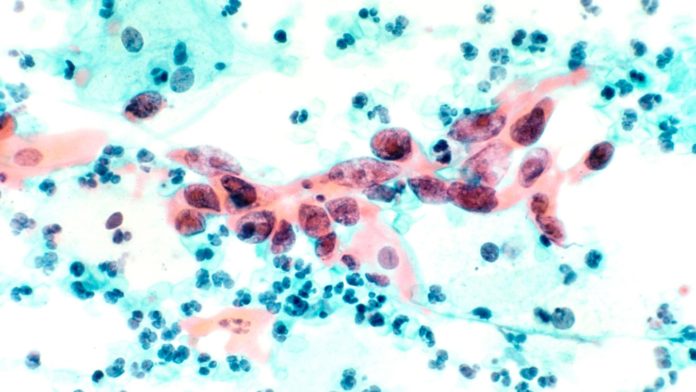
The Pap smear involves scraping clumps of cells from the back of the cervix and studying them for abnormalities indicating precancerous conditions.
Alternatively, there is the HPV test. A machine-based exam, the process is less invasive than the Pap smear, and its purpose is to find high-risk strains of the virus before they develop these dangerous abnormalities.
HPV is one step ahead of the Pap smear
For this study, the women involved were segmented into two groups. Around half of the women were initially tested using the HPV test, and if the results were negative, these women went on to take both the Pap smear and the HPV test four years later.
The remaining half made up the control group, who received the Pap smear at the start. If the results came back negative, they were tested again two years later, and if negative once more, they were tested with both methods at the four-year mark.
Researchers found that after four years, the HPV-negative group were less likely to have evidence of changes that lead to cervical cancer – more specifically, the presence of cervical intraepithelial neoplasia.
By contrast, in more than 300 women, the Pap smear missed these signs of precancerous conditions.
“These results have demonstrated that primary HPV testing detects cervical neoplasia earlier and more accurately than (the Pap smear),” according to the team.
Co-testing with both may be the safest bet
In his comments to ABC, Mark Spitzer from the Center for Colposcopy said that we shouldn’t be so quick to ditch the Pap smear, advocating co-testing instead.
“We really can’t answer the question around whether co-testing is better than either alone,” says Spitzer. “We know that the HPV test missed some early cancerous lesions in some women. In fact, at the conclusion of the study, all HPV-negative women were tested with the Pap smear, which led to finding additional cases of pre-cancerous lesions.”
The number of exceptions in the HPV group was low, but for any individual affected, co-testing can mean a world of difference.
“Most women and doctors are not willing to give up this additional impact,” adds Spitzer. “If you’re one of those people, for instance, it’s very significant.”
Still, co-testing is somewhat of a First World luxury, given the costs involved. Poorer countries with little to no access to Pap smear testing could significantly improve their situation by implementing the more cost-effective HPV test instead, as encouraged by the World Health Organization.
“So these implications are important for North America, but they’re really important for the whole world,” says the University of Texas’s Kathleen Schemeler, speaking to CNN. “Cervical cancer is more common in lower-resource settings where people don’t have access to screening.”