Plumping up fat cells in bone marrow may help in the fight against acute myeloid leukemia (AML), according to research from McMaster University’s Stem Cell and Cancer Research Institute.
Researchers studied the effect of a drug used to moderate type II diabetes that induces fat cell production in the bone marrow. In a surprise win-win, not only did the increase in fat cells suppress the cancerous leukemia cells, but it also facilitated the regeneration of healthy blood cells – a resource that’s critically lacking in patients.
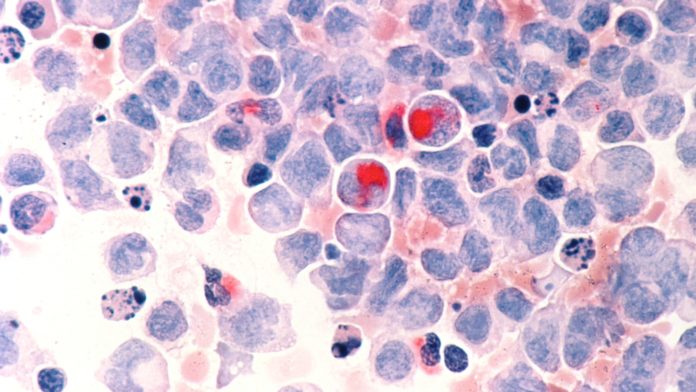
Leukemia starts with blood stem cells that develop abnormally and don’t progress from blast cells into mature red or white blood cells. Eventually, the stagnant blast cells – cancerous leukemia cells that reproduce quickly – overcrowd the healthy cells and prevent them from being able to do their job.
The Leukemia and Lymphoma Society of Canada estimates there are approximately 43,335 individuals living with the disease in Canada.
A toxic environment for toxic cells
As opposed to killing the leukemic cells through chemotherapy, the team theorized that changing the environment around the cells would be more effective.
“Everyone thinks about killing the disease, but the real problem for patients is they become anemic,” said co-author Mick Bhatia, speaking to the CBC.
Anemia and infections are a result of insufficient levels of healthy blood cells and are leading causes of hospitalization and death among the leukemic population.
“These traditional approaches have not delivered enough new therapeutic options for patients,” says lead-author Allison Boyd. “The standard-of-care for this disease hasn’t changed in several decades.”
Have the stars aligned for those in need of treatment?
Over three and a half years, they replicated how this treatment might work in humans by transferring the disease into mice and studying the effect of the drug. Even with a dosage much lower than would be prescribed for a diabetes patient, they found it effective, so side effects will likely be only minimal.
“The fact that we can target one cell type in one tissue using an existing drug makes us excited about the possibilities of testing this in patients,” says Bhatia.
“We can envision this becoming a potential new therapeutic approach that can either be added to existing treatments or even replace others in the near future. The fact that this drug activates blood regeneration may provide benefits for those waiting for bone marrow transplants by activating their own healthy cells.”
Bhatia believes it will probably be another two or three years before clinical trials begin because of funding and approvals, but this could be a landmark moment for researchers and patients alike.