Antibiotics continue to be routinely used to treat US children under 2 years of age suffering from bronchiolitis, despite recommendations against this practice issued over a decade ago.
That’s the lead finding of a new study by Canadian and American researchers who have raised concerns about medical practitioners putting young patients at risk while simultaneously contributing to antibiotic resistance. In the vast majority of cases, bronchiolitis is caused by a viral infection, so antibiotics are of no help.
Many patients received antibiotics despite minimal bacterial threat
The team analyzed emergency department (ED) data between 2007 and 2015 collected as part of the National Hospital Ambulatory Medical Care Survey. This nationally representative survey is undertaken annually by the Centers for Disease Control and Prevention, involving around 300 randomly selected EDs and 30,000 visits.
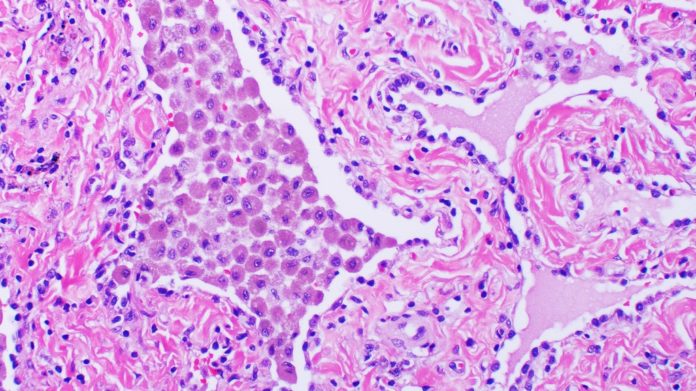
Bronchiolitis is the leading cause of hospitalization for children less than 1 year old in the US. The condition develops when the bronchioles (small airways that lead to the lung) become inflamed and congested with mucus.
The study results showed that one in four children treated for bronchiolitis received antibiotics and there was no significant reduction in prescription rates over the study period. Of all the patients who were prescribed antibiotics, 70% had no documented bacterial infection. That’s close to 18% of pediatric bronchiolitis cases being treated using antibiotics.
In 2006, the American Academy of Pediatrics (AAP) published a report advocating for the removal of antibiotics as a routine treatment for bronchiolitis if bacterial infection is undocumented. In that report, the AAP stated that kids with bronchiolitis have less than a 1% chance of developing an invasive bacterial infection, so it was only logical to remove antibiotics from the equation, bar exceptional circumstances.
Further, they found that the type of hospital involved was an independent factor. If a hospital was neither a teaching hospital nor a pediatric hospital, the chances of this unfortunate practice occurring were higher.
Despite its rarity, the study authors believe that the ongoing inappropriate use of antibiotics is “driven by concern for a concomitant bacterial infection”. They attribute this to a delay in translating guidelines to clinical practice and have emphasized the need to put greater effort into educating health care professionals and the public about antibiotic misuse.
Antibiotics: A blessing and an ever-growing curse
Antibiotics have multiple drawbacks. While these medicines are at work, they have the potential to eliminate too much ‘good bacteria’ along with the bad, which can lead to unintended consequences like diarrhea and infections.
Previous research has shown that approximately 70,000 ED visits happen every year in the US because of adverse reactions to antibiotics in patients aged 19 or under. The same study reported that kids under 2 years of age – the same demographic in this new paper – are most at risk.
Liberally prescribing antibiotics also contributes to antibiotic resistance – “one of the biggest threats to global health, food security, and development today,” according to the World Health Organization.
The more these medicines are in circulation, the higher the probability of bacteria developing resistance to their effects, creating a major health hazard. Examples of antibiotic-resistant superbugs include Staphylococcus aureus, better known as MRSA, and Vancomycin-resistant Enterococci (VRE)
“For parents and other caregivers of children, these findings are a reminder that while antibiotics save lives when used appropriately, antibiotics also can harm children and should only be used when needed,” says lead author, Maribeth C. Lovegrove.
“For healthcare providers, these findings are a reminder that adverse effects from antibiotics are common and can be clinically significant and consequential for pediatric patients.”